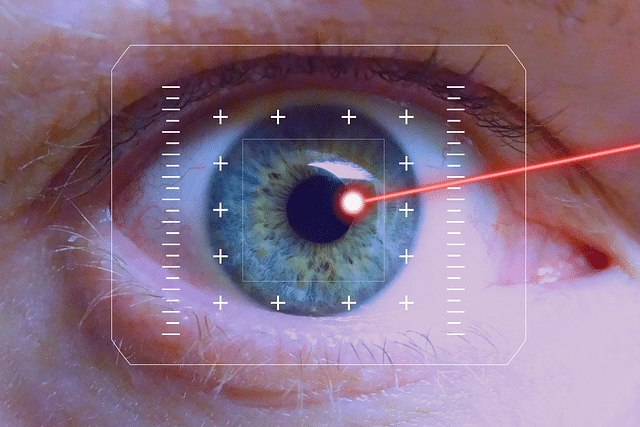
So far so good. The laser procedure, a peripheral iridotomy, that I had today did not cause the fluid in my eyes to boil and my eyes did not explode. There was almost no chance that such a thing could happen. The micro-wattage of the laser used in such procedures does not have enough power to boil your eyeball. But more powerful lasers could make your eyeballs explode. I think about these kinds of things.
A few weeks ago, in September, I went in for a routine eye examination with my optometrist. She told me I had narrow angles. Then two weeks later I went to my ophthalmologist. He verified the diagnosis and we discussed my options. I decided to have both eyes done at the same time. There is no slicing and dicing of anything so the likelihood of infection is very low. I would not have lens replacement or cataract surgery done one both eyes at the same time. After a week or so my insurance company weighed in with a thumbs up on covering the cost of surgery. We scheduled the surgery.
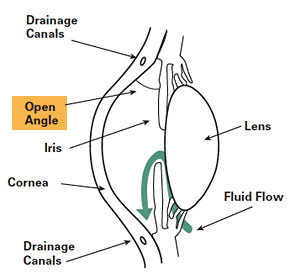
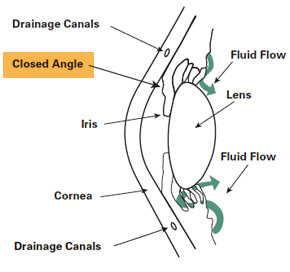
This refers to space between the iris the amount of drainage area in the eye. If you have a narrow angle between the iris and the cornea it is more likely for drainage from the eye to to be blocked when pressure builds within the eye and pushes the iris outward or when the iris is bunches together as the pupil dilates. Essentially the iris can float forward and block the drainage mesh. If this happens the pressure inside the eye can suddenly build and neural damage and loss of sight can occur.
Essentially what I had was a preventive procedure. This should forestall or prevent acute narrow angle glaucoma from developing.
Why Would I Do This?
So why would I undergo this procedure if I did not absolutely have to do it?
- If my narrow angle condition becomes an acute narrow angle glaucoma attack I could lose some or all eyesight in that eye. This significantly decreases the chance of my having an attack.
- I am also borderline or pre-diabetic. This increases my chances of developing eye problems, especially glaucoma.
- My brother developed blindness in one eye and never found out why. He was amblyopic in the eye that eventually developed blindness. Amblyopia does not cause blindness. He passed away in 1998. I never asked him any detailed health questions. Great strides have been made in diagnosis and treatment since then. Also he did not have any health insurance, lived in poverty, and so sought out health care only when in crisis. There are lots of unanswered questions here, but I suspect something narrow angles might have been involved. We both had brown eyes. I know that brown eyes do have a greater chance of developing cataracts.
- Glaucoma sneaks up on you. Once you notice symptoms it is too late to prevent damage.
- I have good health insurance.
The Procedure
I could eat and drink normally prior to the procedure. I did fill a prescription for eyedrops to be used four times a day for five days after surgery.
The procedure was outpatient. I filled out a few forms and paid my co-payment. Waited in the waiting area and read Real Simple.
Then I was called into an area containing several identical recliners. This area was just beyond several alcoves and halls that seemed to be for different types of surgical procedures. I was twice asked by different people, why I was there. This seemed weird at first, but in retrospect it is a very good question to verify expectations, understanding, and state of mind. Four different nurses and techs collected my health history, verified my identity via a wrist band three different times, then numbing eye drops were administered, then a drop to constrict my pupils was administered, then another medication to reduce eye pressure was dropped in my eyes.
They warned me I would get a headache.
I was asked if I wanted a drink before the procedure while the medications took effect. I opted for a diet soda.
My blood pressure was taken.
The surgery room looked a lot like a a normal eye exam room. The laser equipment was smaller than”regular” equipment in an optometrist’s office. I was given more numbing drops in the procedure room. The chair, yep the procedure is done while you are sitting, was stationary, and the laser table was moved toward me. The room is darkened. The nurse and doctor vocally verified settings, positions, levels and such. I put my chin and forehead in the rests of the same kind of guide used in regular eye exams. I look at a green light next to the laser to keep my eyes focused forward. A lens with goop of some sort on it is placed against my eye. The procedure is the same for both eyes.
The right eye took three light bursts with the laser to create a small hole through the outer edge of the iris. The left eye took five or six laser bursts. These holes will allow fluid to have an exit point should the narrow angle close and pressure build up.
The actual procedure on both eyes took less than five minutes. By that I mean the surgeon was in the room with the nurse and I for less than 5 minutes.
This in no way seemed like the Ludovico treatment in A Clockwork Orange. I had wondered about that.
My Experience
I thought I would see a bright white light, but what I experienced was seeing a red mesh pattern that had to be the blood vessels at the back of my eye. Why I saw them, I don’t know. There was some micro-momentary pain in the right eye. Mainly there was discomfort.
After the doctor left, the nurse rinsed out the goop from my eyes and I was escorted back to the recliner area where I was to hang out for approximately 30 minutes so they could measure the pressure in both eyes. The bits of iris they zapped off could raise the eye pressure if they lodged such that they blocked fluid flow.
My sight was very blurry. I didn’t like the overhead florescent lights in the “recliner” area, so I put on sunglasses. It helped. I looked way cool.

My pressure was fine, and the nurse made sure that I had scheduled a followup appointment.
I did develop a headache, but not a terrible one.
My right eye continued to hurt, but not badly, for the rest of the day.
Summarily, the procedure was short and not at all bad, all things considered. Given the significant statistical odds of developing a condition that would destroy my eyesight, having this procedure was a no brainer for me.
I, of course, am not recommending anyone else decide whether to have an iridotomy based on anything I have said. I am sharing this so that persons who decide to have the procedure might know what my experience was, and to let my friends know what this experience was like for me.
I am truly in awe of how medical technology has developed in my lifetime. Surgery was the only procedure to treat this condition prior to the early 1980s. Laser technology has advanced significantly from the use of argon lasers to Nd:YAG lasers. The use of lenses and gels to reduce damage that can occur from heat during treatments has also been developed. Laser iridotomy is a very safe treatment and that safety has made preventive treatment a reasonable option in people deemed to be at risk of having a narrow angle attack.